What does WHO4, WHO 5, WHO 6 and the literature say about the use of CASA?
Computer aided sperm analysis is capable of measuring sperm parameters such as motility, morphology, vitality etc. quantitatively and accurately. The question is to what extent does WHO 4, 5 and 6 accept CASA technology as both a diagnostic and a clinical tool?
The World Health Organization Manuals on sperm analysis and quality assessment date back to 1980. Six versions on sperm analysis by WHO have since been published including the last version, WHO 6, appearing in July 2021 (Fig. 1). The manuals have often mistakenly been used by many laboratories and IVF centres in predicting fertility instead of being used as a practical guide to assess semen quality and an indication of the health of the patient/donor. Table 1 shows the most important semen characteristics and the adjustment of the values over 40 years. Determination of the actual cut-off values for good quality semen has predominantly been based on scientific research up to WHO 4 (1999) and it was suggested that for WHO 5 (2010) the emphasis shifted to outcome based. However, this has been criticised by many for good reason. Despite shortcomings, the WHO 6 (2021) manual has been considerably improved under the editorship of Lars Bjorndahl (Fig. 1).
Fig. 1: The World Health Organization (WHO) manuals on: WHO laboratory manual for the examination of semen: WHO 4 (1999), WHO 5 (2010) and WHO 6 (2021).
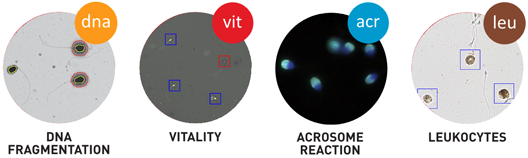
Most of the WHO laboratory examinations for semen analysis have been based on manual assessment of different sperm traits such as motility grades as well as the determination of the percentage normal sperm as examples. There is a large body of information that manual assessment of these sperm traits remain subjective and prone to many errors and producing a large coefficient of variation. In contrast, particularly in the last decade some CASA systems such as the Sperm Class Analyzer has automated modules for vitality, fragmentation, acrosome reaction and leukocyte count apart from the well-established sperm concentration/motility and morphology CASA modules.
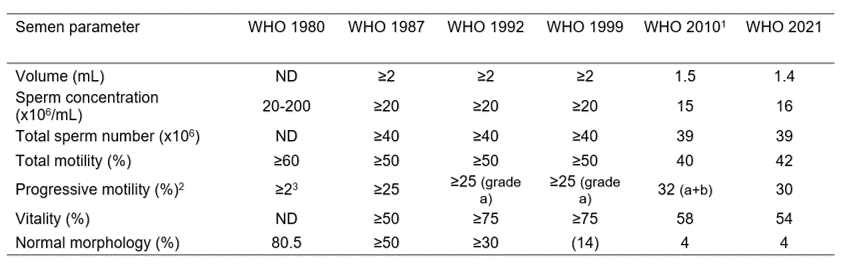
Table 1: Cut-off reference values for semen characteristics as published in consecutive WHO manuals.
In view of the above points raised, what is the status of CASA related to the WHO manuals for semen analysis? In WHO 4 (1999) CASA is acknowledged as being able to provide high precision and determine sperm concentration within a certain sperm concentration range and provide quantitative data on different kinematics. However, there is concern about standardization among systems. In WHO 4 there is no specific recommendation regarding the diagnostic use of CASA despite citing papers (1993-1995) that showed relationships between progressive sperm motility and in vitro fertilization rates.
The section on CASA has been considerably expanded in WHO 5 (2010). Apart from the issues raised in WHO 4 (1999) it suggests that the use of fluorescent DNA stains as well as tail-detection algorithms allow sperm concentration and the percentage motile sperm to be more accurately determined. It furthermore suggests specific methodologies to be used to assess sperm motility and affirms CASA kinematic terminology to be used. In addition, WHO 5 also provides supportive information on the use of CASA sperm morphology analysis. Some references are provided showing sperm morphology to be significant predictors of fertilization rates in vitro. Yet despite the scientific/clinical evidence WHO 5 suggests that much more research is needed to demonstrate the benefit of CASA for clinics.
CASA has been further elaborated in WHO 6 (2021). Caution is again presented in terms of the problems related to debris in semen that may be detected as immotile sperm. However, the problem relates to most CASA systems using negative phase contrast microscopy for sperm concentration and sperm motility determination which will not distinguish between sperm and background particles. This will lead to an over estimation of sperm concentration and an under estimation of the percentage sperm motility. WHO 6 does not acknowledge that some major CASA systems such as SCA (Microptic SL) uses positive phase contrast microscopy which clearly distinguishes between sperm (white particles) and background particles (grey and black particles). In addition, WHO 6 also omits the previous suggested use of fluorescence DNA stains for sperm concentration and motility determination and present further options in modern CASA systems.

Modern CASA system (SCA) showing all the hardware components that can be used and interfaced.
It is encouraging to observe that WHO 6 now incorporates CASA for evaluating sperm functional aspects such as hyperactivation (HA). Hyperactivation has been shown to be related to fertilization and live birth outcome in humans and animals. By using a combination of kinematic parameters the percentage hyperactivation can be established (associated with potential fertility >20% HA) and this is not possible by means of manual analysis. This is commonly performed by head centroid tracking of sperm but more emphasis should be placed on flagellar analysis (suggested by WHO 6) since it is the flagellum that propels the sperm and not the sperm head.
WHO 6 also omits the value of CASA in estimating sperm mucous penetration (SMP). With SMP a combination of CASA kinematic parameters has been established to assess the ability of sperm to swim through a viscous medium such as seminal plasma and cervical mucous.
WHO 6 also expands on the importance of sperm morphology assessment using CASA and elaborates on the pitfalls and measures that need to be taken into consideration. It clearly states that CASA assessment of sperm morphology shows greater objectivity, precision and reproducibility than manual methods. However, WHO 6 omits the importance of CASA being able to accurately, quantitatively and very rapidly measure sperm morphology indices such as the teratozoospermia (TZI) and multiple anomalies index (MAI). These indices refer to the number of abnormalities per sperm or abnormalities of the sperm population and these indices may better predict sperm abnormality than just the percentage sperm motility.
Unfortunately, WHO 6 does not provide further information on the CASA automated modules relating to sperm vitality, fragmentation, leukocyte count and a further sperm functional test, the acrosome reaction. These have been developed as part of CASA systems and need to be given the recognition they deserve:
In conclusion it appears that more recognition has been given to CASA since WHO 4 with some encouraging new sections in WHO 6. It is erroneous though that despite the major developments and advantages of CASA in providing more objective and quantitative information on sperm quality and functionality far too little attention is devoted to it and instead the emphasis remains on subjective manual analysis. Fortunately, CASA seems to be extensively and increasingly used in Andrology laboratories and both smaller and major clinics and IVF centres across the globe. It can only be hoped that these centres and research units further show the advantages of using a technology that has proven itself not only in the research environment but also the diagnostic and clinical spheres.
Prof Gerhard van der Horst (PhD, PhD)
Senior Consultant
MICROPTIC S.L.



Leave A Comment