New ventures in our understanding of sperm functionality
In 2016 I wrote a blog on standardization of semen analysis in humans but with the emphasis on reviewing sperm motility analysis since the 1600’s until 2016. I showed the importance of standardization of quantitative semen analyses and the power of CASA in assisting to better define sperm motility, morphology, vitality, fragmentation and sperm functional tests. New questions emerge: Firstly, has anything changed in CASA and related analyses in sperm motility in the last few years, particularly in relation to ART?
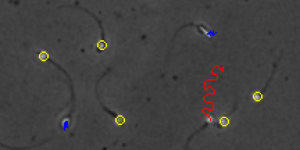
During the last few years it has become more apparent to users of WHO 2010 that it is to inform us about the assessment of sperm quality and not tell us about the fertility of the patient. Secondly, there has been an increased awareness that sperm functionality is likely to inform us better about which sperm will fertilize the oocyte. Sperm functional tests such as sperm (cervical) mucus penetration and hyperactivation have now become central in testing the ability of sperm to fertilize the oocyte. These tests rely on the measurement and quantification of important motility characteristics. Moreover, CASA systems such as SCA now routinely quantify these two aspects by using certain sperm kinematics and cut-off points exist in terms of CASA analysis. It seems that when >5 million sperm/ejaculate pass the sperm mucus penetration test (as measured by SCA CASA) it refers to sperm that are likely to reach the oviduct and fertilize the oocyte. Similarly, when about 20% of sperm become hyperactivated (essential to fertilize oocyte) as measured by CASA, there is a very high chance that fertilization will take place and also that there will in fact be a live birth outcome. Moreover, when these tests are combined with CASA vitality analyses and hypo-osmotic swelling and CASA DNA fragmentation analysis, it is particularly useful in the selection of sperm for ICSI.
What does this mean in the everyday practise of IUI/IVF/ICSI?
The problem in the clinical laboratory relating to ART is that clinicians want an ideal technique to select a sperm that will be best for ICSI. Despite IMSI and other techniques which rely on a single sperm characteristic, it does not exist in reality. The ability of sperm to fertilize the oocyte is dependent on many factors. For example, sperm may have good motility and even acceptable morphology yet there may be abnormalities in terms of the chromatin packaging and sperm fragmentation. So what needs to be done in the clinical laboratory? Firstly, a little bit more patience is required in terms of understanding your patient. While it may not always be practical in the clinical setting there is a great need to understand the patient in terms of semen analysis and sperm functionality (at least two semen analyses over six weeks including sperm functional testing, mucus penetration, hyperactivation, DNA fragmentation).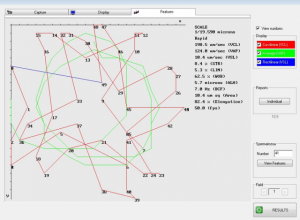
Several publications in the last 18 months have shown that sperm functionality in the second ejaculate a few hours after one three days after abstinence is functionality much better. This will assist the embryologist better to not only understand the patient better but to select sperm for ICSI. Which other factors are important with the second ejaculate? Media can be used that contain natural stimulants for sperm capacitation including hyperactivation. Hyperactivated sperm can be easily selected (microscopic inspection) when motility is low and osmotically swollen sperm represent good sperm membranes for ICSI selection.
Accordingly, two approaches can be implemented using SCA CASA motility and can be implemented before IUI, IVF, ICSI. One example will suffice: Use washed sperm from second ejaculate shortly after first, stimulate with a capacitation medium and then select sperm that become hyperactivated (can be visually detected). The rationale is that correlations can be found between CASA analysis, manual selection of a hyperactivated sperm and outcomes (fertilization or clinical pregnancy).
This blog emphasises the need for analysing sperm using quantitative methods such as CASA and determine sperm functionality of your patient. A simple ICSI approach may be to select a hyperactivated sperm but only after first tests have shown low levels of fragmentation and sperm mucus penetration.
Prof Gerhard van der Horst (PhD, PhD)
Senior Consultant
MICROPTIC S.L.


Leave A Comment